Prof. Shahzad Shams presently works as Head and Professor of the Neurosurgery Department at Lahore General Hospital, LGH, Lahore.
Childhood Brain Tumors
Pediatric Neurosurgery by prof. Shahzad provides individualized care for infants to young adults and encompasses the full range of neurosurgical disorders affecting a child’s brain or spinal cord. Prof. Shahzad leads the dedicated pediatric team consisting of neurosurgeons, anesthesiologists, and specialized nurses.
In 2010-11 Omar hospital was ranked as the best pediatric hospital in Lahore for neurosurgery and amongst the top institutions overall, nationally. Due to the neurosurgery team’s clinical expertise, integration with neuroscientists.
And professional support from an array of family-centered specialists like pediatric therapists, on-site child education and recreation therapy, the Pediatric Neurosurgery program by Prof Shahzad has earned a national reputation for delivering the highest standard of family-focused care.
This center has the most advanced surgical facility in the country, designed exclusively for pediatrics, allowing the pediatric neurosurgical team to tackle even the most formidable of diseases and conditions.
Pediatric Endoscopic Brain Surgery
Cranial Endoscopic Procedures
1. Endoscopic Pituitary Surgery And Craniopharyngioma Surgery
Endoscopic pituitary surgery and Craniopharyngioma surgery also called Transnasal Transsphenoidal Endoscopic Pituitary Adenoma Surgery is performed through a natural nasal air pathway through the nose without any incisions unlike the conventional microscopic surgery performed with an incision made under the upper lip or inner aspect of a nostril.
Endoscopic surgery does not require the use of a metallic Transsphenoidal retractor that is used for conventional Microscopic Transnasal Transsphenoidal Pituitary Tumour surgery. A 4-mm endoscope is placed in front of the tumor in the sphenoidal sinus and the tumor is removed with specially designed surgical tools.
Postoperative nasal packing is not necessary, and postoperative discomfort is minimal.
Most patients are able to go home the following day. The optical advantages of an endoscope (such as a wide-angle panoramic view, an angled view by angled lens endoscopes, and a view in the tumor removal cavity) enhance tumor removal even in complex cases of bulky tumors.
Advantages of Endoscopic Pituitary Surgery and Craniopharyngioma surgery
- With this newly developed minimally invasive technique, pituitary tumors can be removed through the patient’s natural nose.
- This procedure does not require sub labial or nostril incisions and eliminates the need for occlusive postoperative packing used with the conventional procedures.
- This method is minimally invasive because it directly approaches the tumor through the patient’s nostril thus eliminating facial swelling, decreasing postoperative pain, and making recovery quicker.
- The procedure is innovative because it utilizes endoscopic technology to improve visualization of the pituitary gland, the tumor, and other anatomical structures.
- Most patients can go home the day following their surgery. Endoscopic minimally invasive keyhole technique for tumor excision through the nose without any incision and a hospital stay 24 hours.
2. Endoscopic Minimally Invasive Keyhole Surgery For Management Of Intraventricular Brain Tumors
Endoscopic Management Of Intraventricular
Brain Tumors
The cerebral ventricles are chambers within the brain that contain a clear-colorless fluid called cerebrospinal fluid (CSF). CSF serves as an excellent medium for endoscopy given clarity and space. Since many varieties of brain tumors can occur in the ventricles, biopsy is commonly recommended in order to define the best type of therapy.
Conventional procedures for tumor biopsy involve either a needle biopsy using a frame attached to the skull or an open surgical procedure. Brain tumors situated in the intraventricular compartment are amenable to an endoscopic biopsy or resection.
Endoscopic Tumor Surgery
The procedure is performed through a small incision (approximately 1 inch) behind the hairline. From this site, the endoscope is inserted into the ventricular compartment of the brain and then navigated toward the tumor.
The tumor is readily identified due to the difference in appearance from the surrounding tissue. Biopsy forceps are then used to sample the tumor. Because direct vision is being used, samples can be selected avoiding any small blood vessels or other important structures within the ventricle, features that cannot be done with standard “closed” needle biopsies.
The endoscope is then removed and the wound is closed. The procedure is performed in approximately 30 minutes and patients can return home the following day. Endoscopic biopsy for intraventricular brain tumors avoids many of the inherent risks associated with conventional surgical approaches.
Because these tumors are typically situated deep within the brain, the ability to approach these tumors with a minimally
Treatment
Endoscopic Minimally Invasive Keyhole Surgery For Tumor Excision Through A Small Opening Of 2cm And Short Hospital Stay.
Pediatric Or Childhood Brain Tumors
Brain tumors are among the most common childhood malignancies and they vary widely in their type, location, and growth rate. Brain tumors are the most common solid tumors in children and account for 20% of all childhood malignancies.
Symptoms
Brain tumors can cause multiple symptoms depending on their location, its rate of growth, and the age of the child. Tumors in any location can cause increased pressure within the skull causing the child to experience headaches, nausea, vomiting, and double vision.
In infants, the increased pressure may cause excessive, rapid head growth. Tumors located in the back of the brain (posterior fossa) can also cause unsteadiness and difficulties with speech and swallowing.
Tumors located in the top part of the brain (supratentorial) can cause seizures (involuntary convulsions with or without loss of consciousness) or weakness of the arms or legs. Tumors located near the base of the brain (suprasellar) can cause visual problems as well as hormonal imbalances that can lead to several conditions including growth disorders.
Diagnosis
When a child develops symptoms that are suggestive of a brain tumor, the mainstay of establishing the diagnosis is through imaging of the brain. This is done by either a CT scan or MRI Scan.
While these types of images will demonstrate whether an abnormal mass is present in the brain, in only a few cases will this be enough to establish what type of a mass it is. Aside from brain tumor, abnormal masses in the brain could be caused by infection, bleeding, or a long-standing congenital abnormality.
In most cases, some form of surgery is required in order to remove a sample of tissue. By analyzing the tissue, one can know for sure whether the mass is a tumor and, more importantly, exactly what type of tumor it is.
Treatment
The treatment of brain tumors varies greatly and is dependent by several factors including the size and location of the tumor, the age of the child, and the expected growth rate of the tumor. The main modalities of treatment are surgery, radiation therapy, and chemotherapy.
Surgery
Latest Technique Is Endoscopic Surgery Done Through Nose Or A Endoscopic Minimally Invasive Keyhole 2cm Opening With Short Hospital Stay
Surgery for brain tumors can be performed for different purposes, depending on the type, size and location of the tumor. The possible goals of surgery may be one of or any combination of the following:
1. To remove as much of the tumor as is safely possible. One of the great difficulties in removing brain tumours, as opposed to tumours in other locations in the body, is that extreme care must to be taken to try to prevent harm to the very delicate brain tissue. For most childhood tumors, the prognosis is generally better if the tumour can be either totally or near-totally removed. Therefore, surgery remains the mainstay of therapy for the majority of childhood tumors.
2. To remove enough of the tumour to improve the patient’s symptoms. For example, if a large tumor is causing increased pressure in the skull, or weakness of the arms or legs, or seizures, then surgery on the tumour may help relieve these symptoms.
3. Provide a tissue sample of the tumour. This tissue sample is analyzed by pathologists and this will tell the surgeon what type of tumour it is and, possibly, how aggressively it might be expected to behave. This will also help decide what type of treatment is needed.
Radiation Therapy
Radiation therapy involves passing high energy radiation through the body. Radiation slows rapidly growing tissue, like tumours. Radiation therapy is often used in conjunction with surgical therapy.
The dose and timing of the radiation regimen depends on the type of tumor. In some cases, radiation might only be applied to the local area of the tumor, whereas in other cases, an additional radiation dose might be given to the entire brain and spinal cord to try to prevent the tumor from seeding via the spinal fluid.
Because of the fear that radiation therapy may adversely effect the very young, developing brain, it is usually not performed in infants and very young children. Potential side-effects of radiation therapy include hair loss, nausea, vomiting, fatigue, and local skin irritation.
Chemotherapy
Chemotherapy involves giving very strong medications (directly into the bloodstream or occasionally as pills) that preferentially destroy tumor cells. There are numerous drugs that may be used for various types of brain tumors.
Although some chemotherapy drugs can improve the survival of children with certain brain tumors, the drugs themselves can have substantial side-effects, including severe nausea, hair loss, and risk of infection.
Types of Brain Tumors
There are several different types of brain tumors that can affect children. Only some of the more common ones will be discussed here.
Craniopharyngioma
These tumors are located near the optic nerves and the pituitary gland, so they frequently cause visual problems and hormonal imbalances. The standard therapy for these tumours is surgery, attempting to remove as much of the tumor as is safely possible.
Total removal of the tumor is very difficult and, because of its location, visual disturbances and hormonal imbalances are not uncommon after surgery. Radiation therapy is occasionally used if substantial tumour remains after surgery or if the tumor shows re-growth.
Astrocytoma
Astrocytomas are tumors that can either be low-grade or high-grade. The low-grade variety is commonly found in the back of the brain (posterior fossa) and these account for approximately 10% of all childhood brain tumours.
They may, however, also be located in the top of the brain (supratentorial). Surgical removal of these tumors, especially in the posterior fossa, carries an excellent prognosis for complete cure.
The overall prognosis for these tumors is very good. High-grade Astrocytomas are most commonly located in the top of the brain (supratentorial). Treatment usually consists of a combination of surgery, chemotherapy, and radiation. These are quite aggressive tumours and the prognosis is much worse than for the low-grade variety.
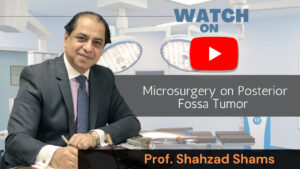
Ependymoma
Ependymomas most commonly occur in the back of the brain (posterior fossa). Therapy consists of surgery, attempting to remove as much of the tumour as is safely possible, and radiation therapy.
Medulloblastoma
Medulloblastoma is another common tumour of the back of the brain (posterior fossa).Treatment initially consists of surgical removal. This is usually followed by radiation therapy, which frequently involves radiation to the entire brain and spinal cord to prevent the spread of the tumor to another location. Depending on the extent of the tumour, chemotherapy may also be considered.
Brainstem Glioma
The brainstem is the central area of the brain, where all the nerve fibers that travel between the brain and body meet. Tumours that arise in this delicate location are usually gliomas that can either be high-grade or low-grade
High-grade brainstem gliomas are very difficult to treat. They may be diagnosed based on brain imaging alone. Surgical removal is extremely difficult and so therapy is usually confined to radiation and, sometimes, chemotherapy.
Low-grade brainstem gliomas are quite different and sometimes need no urgent therapy. They can sometimes simply be watched with repeated brain imaging. It is not uncommon for these to remain unchanged for many years.
Tumors in the brainstem are particularly prone, due to their location, to obstruct the flow of the brain’s natural fluid. This causes a build-up of fluid in the brain (hydrocephalus) and increased pressure in the skull.
The treatment for this can involve either placement of a silastic tube (shunt) to drain the fluid into the abdomen or the creation of a separate hole in the brain to divert the tumour obstruction (endoscopic third ventriculostomy).